ABSTRACT
Purpose:
To determine the reliability of swept- source optical coherence tomography in cases in which soft contact lenses cannot be removed when acquiring biometric measurements.
Methods:
Eight subjects were included and only one eye per participant was analyzed. Each eye was measured six times by swept-source optical coherence tomography with the IOLMaster 700 instrument (Carl Zeiss Meditec, Jena, Germany). Axial length, central corneal thickness, anterior chamber depth, lens thickness, and keratometric measurements were evaluated for the naked eye and while wearing soft contact lenses of three different powers (-1.5, -3.0, and +2.0 D).
Results:
There were statistically significant changes in axial length, central corneal thickness, anterior chamber depth, and keratometric measurements with soft contact lenses as compared to the naked eye (p<0.001). However, there were no significant differences in lens thickness outcomes between the naked eye and while wearing the three soft contact lenses (p>0.5). The changes in axial length, central corneal thickness, and anterior chamber depth were lens-specific and dependent on the thickness of the lens used.
Conclusions:
Sept-source optical coherence tomography based lens thickness measurements while wearing soft contact lenses are comparable to those of the naked eye. However, the thickness and the optical design of the soft contact lens may lead to significant differences in the axial lengh, central corneal thickness, anterior chamber deph, and keratometric measurements.
Keywords:
Tomography, optical coherence; Contact lenses; Biometry
RESUMO
Objetivo:
Determinar a confiabilidade da tomografia de coerência óptica de varredura em casos especiais em que lentes de contato gelatinosas não podem ser removidas ao realizar medições biométricas.
Métodos:
Oito indivíduos foram incluídos e apenas um olho por participante foi analisado. Cada olho foi medido seis vezes por tomografia de coerência óptica de varredura com o instrumento IOLMaster 700 (Carl Zeiss Meditec, Jena, Alemanha). O comprimento axial, a espessura central da córnea, a profundidade da câmara anterior, a espessura da lente e as medidas ceratométricas foram avaliados a olho nu e enquanto usavam lentes de contato gelatinosas de três diferentes potências (-1,5, -3,0 e +2,0 D).
Resultados:
Houve alterações significativas no comprimento axial, espessura central da córnea, profundidade da câmara anterior e medidas ceratométricas com as lentes de contato gelatinosas em comparação com as a olho nu (p<0,001). No entanto, não houve diferenças significativas nos resultados de espessura do cristalino entre o olho nu e enquanto usava as três lentes de contato gelatinosas (p>0,5). As alterações de comprimento axial, espessura central da córnea e profundidade da câmara anterior foram específicas da lente e dependentes da espessura da lente usada.
Conclusões:
As medições da espessura da lente baseadas na tomografia de coerência óptica da Sept-source, enquanto usam lentes de lentes de contato gelatinosas, são comparáveis às do olho nu. Entretanto, a es pessura e o desenho óptico da lente de contato gelatinosa podem levar a diferenças significativas no comprimento axial, na espessura central da córnea, na profundidade da câmara anterior e nas medidas ceratométricas.
Descritores:
Tomografia de coerência óptica; Lentes de contato; Biometria
INTRODUCTION
Reliable measurement of ocular biometry is necessary for ocular parametric analysis to assess ametropic progression, identify candidates for refractive surgery, and calculate intraocular lens power. The novel ocular optical biometric IOLMaster 700 instrument, recently developed by Carl Zeiss Meditec (Jena, Germany), is a useful swept-source optical coherence tomography (SS-OCT) device with excellent repeatability and reproducibility for non-contact measurement of ocular biometry and generation of optical B-scans (optical cross-sections) to determine the biometric data of the eye(11 Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg. 2015;41(10):2224-32.
2 Kunert KS, Peter M, Blum M, Haigis W, Sekundo W, Schütze J, et al. Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer vs. partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg. 2016;42(1):76-83.-33 Akman A, Asena L, Güngör SG. Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol. 2016;100(9):1201-5.).
Non-contact devices are popular among both patients and clinicians for measurement of ocular parameters to control myopia progression and for reference in refractive and cataract surgeries. Measurements to estimate axial distances are usually performed with the naked eye. International practice guidelines recommend at least 3 days of contact lens rest before measurement of biometric parameters. In some circumstances, however, patients may wear contact therapeutic or bandage contact lenses, extended-wear contact lenses, or contact lenses used for ocular drug delivery (i.e., dry eye, glaucoma therapy) during this examination(44 Blackmore SJ. The use of contact lenses in the treatment of persistent epithelial defects. Cont Lens Anterior Eye. 2010;33(5):239-44.
5 Maulvi FA, Soni TG, Shah DO. Extended release of hyaluronic acid from hydrogel contact lenses for dry eye syndrome. J Biomater Sci Polym Ed. 2015;26(15):1035-50.
6 Hsu KH, Carbia BE, Plummer C, Chauhan A. Dual drug delivery from vitamin E loaded contact lenses for glaucoma therapy. Eur J Pharm Biopharm. 2015;94:312-21.
7 Moezzi AM, Fonn D, Varikooty J, Simpson TL. Overnight corneal swelling with high and low powered silicone hydrogel lenses. J Optom. 2015;8(1):19-26.-88 Maulvi FA, Soni TG, Shah DO. A review on therapeutic contact lenses for ocular drug delivery. Drug Deliv. 2016;23(8):3017-26.). The effects of contact lens on the reliability of the optical instrument during ocular biometric measurements is of great interest.
The aim of the present study was to assess the reliability of ocular biometric parameters obtained with the IOLMaster 700 using SS-OCT in subjects wearing soft contact lenses to obtain evidence of the reliability of this device in those special cases in which contact lenses cannot be removed when measuring biometric parameters.
METHODS
Subjects
The cohort of this crossover study consisted of a sample of eight normal volunteers, aged 25 to 40 years, with non-pathological eyes. All subjects underwent complete eye examinations that included refraction measurements, screening for ocular and systemic diseases, slit-lamp biomicroscopy, and fundal examination. All subjects were free of ocular pathologic conditions with a photopic pupil diameter of >3.0 mm and best-corrected mono cular decimal visual acuity of 20/20 (0.0 logMAR). Exclusion criteria included tear film abnormalities, amblyopia and/or strabismus, history of ocular surgery, and inflammation. The study protocol was approved by the Ethics Committee of the University of Valencia and performed in adherence with the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects after the nature and possible consequence of the study had been explained.
Optical biometer
The IOLMaster 700 instrument is an optical biometric device for measurement of the axial length (AL), central corneal thickness (CCT), anterior chamber depth (ACD), and lens thickness (LT). Both AL and ACD are measured from the anterior surface of the cornea. Besides, the instrument also provides keratometric values (K1 and K2) and white-to-white distances. This device acquires multiple measurements for each of the various eye parameters via a measurement-capture process and calculates an average value per triggered measurement. The AL measurement was obtained by SS-OCT with a scan depth of 44 mm and resolution of 22 mm. The speed of the length measurement with the IOLMaster 700 instrument allows for acquisition of full-eye length tomograms at 2000 A-scans/s by swept-source biometry and the application of optical B-scan technology to determine the biometric data, allowing for cross-sectional visualization of structures along the visual axis.
Experimental procedure
One skilled operator conducted all experimental procedures. Six consecutive measurements of the right eyes of the subjects were included for analysis. Each measurement was obtained at 4 s after the subject last blinked to allow the tear film to spread over the cornea(99 Montés-Micó R, Alió JL, Muñoz G, Charman WN. Temporal changes in optical quality of air-tear film interface at anterior cornea after blink. Invest Ophthalmol Vis Sci. 2004;45(6):1752-7.), and blinking was not permitted during image acquisition. No other examinations or measurements of the eye involving contact lens were conducted on the day prior to the start of the ocular measurements. Only one eye of each subject was included for analysis to avoid artificially reducing the confidence interval of the limits of agreement(1010 McAlinden C, Khadka J, Pesudovs K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt. 2011;31(4):330-8.). Images of all patients were obtained during the same session.
Measurements of the naked eye with no contact lens were first collected and then repeated with the use of three daily disposable contact lenses made from hilafilcon B (59% water content, refractive index 1.4036, FDA material group II) at powers of -1.5, -3.0, and +2.0 D. The base curve of the lenses at a power of -3.0 D was 8.6 mm with a diameter of 14.2 mm and a center thickness of 90 mm. The IOLMaster 700 was then used to measure AL, CCT, ACD, LT, and keratometric parameters. A minimum of 10 min elapsed between insertion of each of the three contact lens and scanning to obtain the measurements to allow for the contact lens to “tighten” to the cornea or edema, which typically is stabilized within the first few minutes of wear(1111 Weschler S, Johnson MH, Businger U. In vivo hydration of hydrogel lenses: the first hour. Int Contact Lens Clin. 1983;10:349-52.).
Statistical analysis
The results were evaluated using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). There were no important asymmetries or significant outliers in any of the data samples. The normality of all data sets was evaluated with the Shapiro-Wilk test. Repeated measures analysis of variance (rANOVA) were performed to reveal significant differences among measurements for each of the parameters obtained with the device. Prior to the rANOVA, the sphericity assumption was assessed using the Mauchly’s sphericity test. When sphericity could not be assumed, the Greenhouse-Geisser correction was applied. The Bonferroni post hoc test was used for comparisons among the data groups when the rANOVA results revealed significant differences between measurements to determine the significance level of paired differences between the individual lens conditions. A probability (p) value of <0.05 was considered statistically significant in all cases.
RESULTS
Measurements were obtained for all subjects and no corneal disturbances occurred during or after the study.
Axial length, central corneal thickness and anterior chamber depth
The AL measurements (mean ± standard deviation) for each lens condition (i.e., without contact lens and with -3.0, -1.5, and +2.0 D contact lenses) are shown in figure 1A. The rANOVA procedure revealed statistically significant differences in the AL measurements among the four data groups (naked eye and wearing each of the three soft contact lenses) (p<0.001). The Bonferroni post hoc tests for multiple comparisons revealed statistically significant differences among most of the paired comparisons, with the exception of the -1.5 vs. -3.0 D outcomes (p>0.12). Figure 1B shows the differences in AL measurements for each lens with respect to the no-lens (naked eye) condition; that is, when the result obtained wearing each contact lens is subtracted from the measurement obtained for the naked eye.
A) AL measurements (mean ± standard deviation) for the naked eye condition and while wearing the three soft contact lenses (-1.5, -3.0, and +2.0 D). B) AL differences for each lens vs. the naked eye condition.
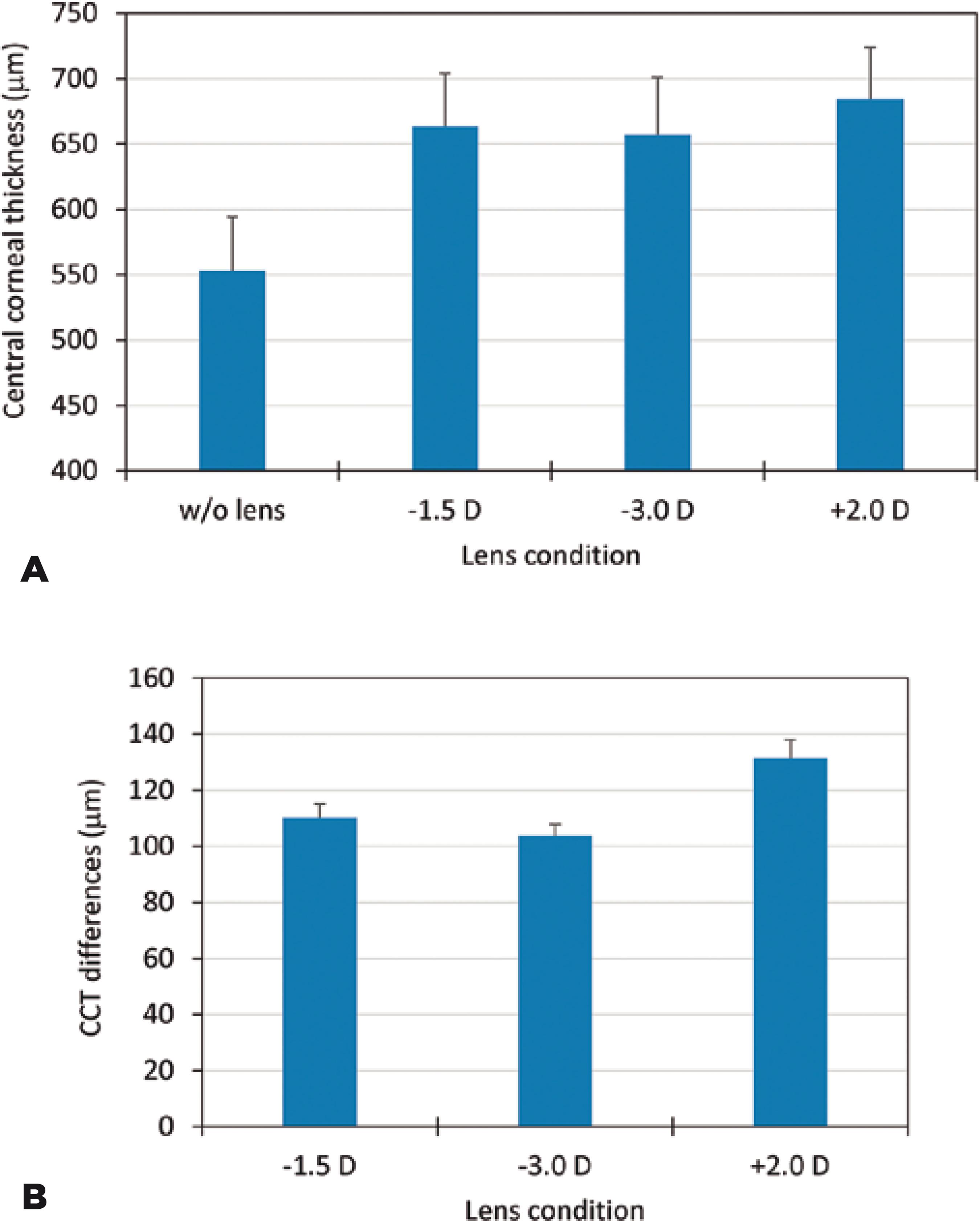
As shown in figures 2A and 3A, the CCT and ACD mea surements were in agreement for each lens condition. The rANOVA procedure revealed statistically significant differences in the CCT and ACD results among the four data groups (all, p<0.001). The results of the Bonferroni post hoc tests revealed statistically significant differences for all of the CCT and ACD paired comparisons, except for the -1.5 D vs. -3.0 D conditions (p>0.05 and 0.95, respectively). Differences in the CCT and ACD values for each lens vs. the naked eye condition are shown in figures 2B and 3B.
A) CCT measurements (mean ± standard deviation) for the naked eye condition and while wearing the three soft contact lenses (-1.5, -3.0, and +2.0 D). B) CCT differences for each lens vs. the naked eye condition.
A) ACD measurements (mean ± standard deviation) for the naked eye condition and while wearing the three soft contact lenses (-1.5, -3.0, and +2.0 D). B) ACD differences for each lens vs. the naked eye condition.
Lens thickness
The LT outcomes for each lens condition are shown in figure 4A. In this case, the rANOVA procedure revea led no statistically significant differences among the four data groups (p>0.5). Figure 4B shows the absolute values of the LT differences for each lens vs. the no-lens condition.
A) LT measurements (mean ± standard deviation) for the naked eye condition and while wearing the three soft contact lenses (-1.5, -3.0, and +2.0 D). B) Absolute value for the LT differences for each lens vs. the naked eye condition.
Keratometric measurements
As shown in Figure 5, there were significant differences in the keratometric measurements (K1 and K2) for the naked eye condition vs. the three soft contact lenses (-1.5, -3.0, and +2.0 D; p<0.001 for all cases and the K1 and K2 measurements).
Keratometric measurements (K1 and K2) for the naked eye condition and while wearing the three soft contact lenses (-1.5, -3.0, and +2.0 D).
DISCUSSION
The aim of the present study was to assess the reliability of ocular biometric parameters of subjects wearing soft contact lenses obtained via SS-OCT with the IOLMaster 700 instrument. It is important to obtain accurate and reliable ocular biometric measurements to provide optimum outcomes when a contact lens is placed on the eye. These results should prove useful to clinicians regarding the clinical performance of this device for ocular biometric measurements.
The results of the present revealed that axial LT mea surements obtained via SS-OCT with an optical biometer are not affected by wearing soft contact lenses (at a significance level of 0.05). However, wearing of contact lens does affect axial AL, CCT, and ACD measurements, as with keratometric measurements, among different lens conditions.
The AL, CCT, and ACD axial distances were significantly increased with the use of the different contact lenses. As shown in figures 1B and 2B, the mean AL and CCT measurements for the three lens conditions (-1.5, -3.0, and +2.0 D) increased by about 110, 100, and 130 mm, respectively, when compared to the naked eye condition. As shown in Figure 3B, with the same lens conditions, the ACD measurements increased by about 100, 90, and 140 mm, respectively. Notably, the differences among the axial distances when wearing a contact lens and the axial distances for the naked eye (no-lens condition) were correlated with the thickness of the contact lens, which explains why the results reported in figures 1B, 2B, and 3B are so similar. According to these results, it seems that the instrument considers both the cornea and the lens to be parts of the same structure, adding both values for the total CCT value. The changes in axial AL, CCT, and ACD distances were directly correlated with the central thickness of the contact lenses, thus yielding a greater change of the positive contact lens. In this sense, the values obtained for the -3.0 D lens are in agreement with the central thickness of the lens (small differences may be obtained because the device seems to consider the contact lens as part of the human cornea by applying the corresponding refraction index when calculating the CCT).
In a similar manner, there were statistically significant differences in keratometric measurements when wearing the contact lenses as compared to the naked eye, which were dependent on the curvature of the fitted soft contact lens and possibly on the method employed by the instrument to obtain the keratometric measurements. In this sense, the double reflection obtained with both the anterior surfaces of the contact lens and the cornea for each of the light spots that the device uses to calculate the keratometric measurements may affect the results. This could be the reason why changes in keratometric measurements are dependent on the lens power, as statistically significant differences were found among all lens conditions vs. the naked eye, as well as each paired lens-to-lens comparison.
There were no statistically significant differences in LT measurements among the lens conditions tested. In contrast to the AL, CCT and ACD measurements, the differences obtained for the LT outcomes when wearing the lenses with respect to the naked eye were small and both positive and negative. In addition, these differences seemed to be randomly distributed around the no-lens value (the absolute values of the differences are shown in Figure 4B), suggesting that the axial LT measurement is independent of the contact lens worn during the OCT assessment, as the same values were obtained with the naked eye. Hence, it would be interesting to determine if the differences in the measurements obtained with and without the contact lens affect the IOL calculations for cataract surgery. The use of some common formulas for IOL calculation (Haigis Suite and Holladay 2) showed that there were no differences in the nominal optical power for the recommended IOL and that the difference in the residual values obtained in both cases was around 0.15 D, much lower than the 0.50 D used for standard IOL measurements.
Although not experienced in the present study, it is important to bear in mind that contact lenses of different negative optical powers can affect the accommodation requirements of the patient when focusing the target used by the device when performing OCT. In this case, different accommodation requirements may be related with different thicknesses and curvatures of the anterior and posterior crystalline lens surfaces, which then affects the LT outcomes obtained by OCT measurements with different contact lenses.
Unfortunately, no previous study has assessed the effect of SS-OCT on biometric measurements of eyes with contact lenses. However, a previous work by Lewis et al.(1212 Lewis JR, Knellinger AE, Mahmoud AM, Mauger TF. Effect of soft contact lenses on optical measurements of axial length and keratometry for biometry in eyes with corneal irregularities. Invest Ophthalmol Vis Sci. 2008;49(8):3371-8.) analyzing on the effect of soft contact lenses on AL and keratometric measurements by partial coherence interferometry (PCI) with corneal irregularities proposed a method to measure the AL of eyes with corneal irregularities or after endothelial keratoplasty while wearing soft contact lens. In this study, dual-beam infrared PCI was used to measure AL and keratometric parameters in 20 subjects while wearing two types of soft contact lenses. Evaluation of this method using two hydrophilic soft contact lenses [a low (38%) and high (58%) water-content polymer) at the same power (-0.50 D) showed that AL increased by about 60 and 130 mm for the low and high water content lenses, respectively. Each soft contact lens increased the AL in a repeatable manner and was reliably detected by PCI. Also, the change in AL measured by PCI corresponded to the OCT-determined contact LT for each lens. OCT was used to measure the contact LT and identify correlations with the change found with the PCI measurement of the AL. Changes in keratometric parameters were also significant when compared to the no-lens condition. The authors concluded that differences in the manufacturing method (cast or soft-molded) and material composition (water content and thickness that correlate with rigidity) might explain these differences. Our SS-OCT results are similar to those with the use of PCI in these former studies.
The elucidation of how the contact lens affects the OCT measurements may help with the use of specially designed therapeutic bandage contact lenses to facilitate epithelial healing in the treatment of several ocular pathologies and postsurgical care. The use of soft contact lenses can accelerate the process of corneal re-epi thelialization and alleviate patient discomfort and the need for some surgeries(1313 Bendoriene J, Vogt U. Therapeutic use of silicone hydrogel contact lenses in children. Eye Contact Lens. 2006;32(2):104-8.
14 Grentzelos MA, Plainis S, Astyrakakis NI, Diakonis VF, Kymionis GD, Kallinikos P, et al. Efficacy of 2 types of silicone hydrogel bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg. 2009;35(12):2103-8.
15 Ozbek Z, Raber IM. Successful management of aniridic ocular surface disease with long-term bandage contact lens wear. Cornea. 2006;25(2):245-7.-1616 Chen D, Lian Y, Li J, Ma Y, Shen M, Lu F. Monitor corneal epithelial healing under bandage contact lens using ultrahigh-resolution optical coherence tomography after pterygium surgery. Eye Contact Lens. 2014;40(3):175-80.). The timing of lens removal is determined by assessment of complete epithetical healing and, thus, lenses should not be worn for longer than necessary due to the potential for secondary infection, but are recommended and should be maintained despite additional measurements, such as ocular biometry.
OCT has also been used as a valid and reliable technique to measure corneal and contact LT in vivo without lens removal(1717 González-Méijome JM, Cerviño A, Peixoto-de-Matos SC, Madrid-Costa D, Jorge J, Ferrer-Blasco T. "In situ" corneal and contact lens thickness changes with high-resolution optical coherence tomography. Cornea. 2012;31(6):633-8.). This method is more convenient for the patient and allows for a more realistic evaluation of the corneal response while wearing a therapeutic contact lenses to avoid any traumatic interaction with the ocular surface during repeated insertion and removal of the lens. Notably, in these cases, the post-lens tear film must be considered, as avoiding such is a potential source of error. In addition, it is necessary to take into account that in OCT measurements, as an optical-based method, changes in the refractive index of the media could adversely affect the thickness measurement. Thus, the refractive index of the polymer of the contact lens should be considered to correct this source of error, especially when the refractive index of the lens is very different from that of the human cornea.
The current study measured only healthy eyes; therefore, these findings should not be applied to pathological eyes or postoperatively altered corneas. Further studies are warranted to assess the reliability of this device in those excluded eye groups. In addition, more types of contact lenses (i.e., rigid and scleral) and different optical powers should be analyzed to evaluate the effects of the measurements with these types of lenses. Despite the limitation of the small number of patients in this study, the results clearly demonstrate that once the physical principles of biometry are understood, greater numbers of samples will not modify the main conclusions of this study. Furthermore, ocular parameters measured in human eyes could be used to assess, for instance, some of the elastic properties of the eye structures by means of the definition and analysis of computational human eye models, which may help to estimate the elastic material properties of the human eye(1818 Cao HJ, Huang CJ, Shih PJ, Wang IJ, Yen JY. A Method of measuring corneal young's modulus. In: Goh J, Lim C, editors. 7th WACBE World Congress on Bioengineering. IFMBE Proc. 2015;52:47-50.
19 Hamilton KE, Pye DC. Young's modulus in normal corneas and the effect on applanation tonometry. Optom Vis Sci. 2008;85(6):445-50.
20 Jones IL, Warner M, Stevens JD. Mathematical modelling of the elastic properties of retina: a determination of Young's modulus. Eye (Lond). 1992;6(Pt 6):556-9.-2121 Aloy MÁ, Adsuara JE, Cerdá-Durán P, Obergaulinger M, Esteve-Taboada JJ, Ferrer-Blasco T, Montés-Micó, R. Estimation of the mechanical properties of the eye through the study of its vibrational modes. PLOS One 2017,vol. 12, issue 9, p. e0183892).
In conclusion, the results of this study confirmed the reliability of the IOLMaster 700 SS-OCT biometer for measurements of AL, CCT, ACD, and LT in eyes wearing soft contact lenses. As the results demonstrate, the CCT measurements obtained with the optical biometer may vary depending on the central thickness of the soft contact lens worn. This change in CCT may affect the AL and ACD measurements. On the contrary, LT measurements are not affected by wearing soft contact lens. Since changes in AL, CCT, and ACD measurements are lens-specific, the central thickness of the contact lens should be taken into account when reporting these values measured with SS-OCT. Finally, keratometric values are affected by the contact lenses and may be dependent on the method employed by the instrument to obtain keratometric mea surements from the light spots reflected on the anterior surfaces of the cornea and the contact lens.
-
Funding: This study was supported by the Spanish Government Grant Explora (SAF2013-49284-EXP), and a University of Valencia research scholarship (UV-INV-PREDOC13-110412) awarded to Alberto Domínguez-Vicent.
-
Approved by the following research ethics committee: Universitat de València (# H1460640726281),
REFERENCES
-
1Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg. 2015;41(10):2224-32.
-
2Kunert KS, Peter M, Blum M, Haigis W, Sekundo W, Schütze J, et al. Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer vs. partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg. 2016;42(1):76-83.
-
3Akman A, Asena L, Güngör SG. Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol. 2016;100(9):1201-5.
-
4Blackmore SJ. The use of contact lenses in the treatment of persistent epithelial defects. Cont Lens Anterior Eye. 2010;33(5):239-44.
-
5Maulvi FA, Soni TG, Shah DO. Extended release of hyaluronic acid from hydrogel contact lenses for dry eye syndrome. J Biomater Sci Polym Ed. 2015;26(15):1035-50.
-
6Hsu KH, Carbia BE, Plummer C, Chauhan A. Dual drug delivery from vitamin E loaded contact lenses for glaucoma therapy. Eur J Pharm Biopharm. 2015;94:312-21.
-
7Moezzi AM, Fonn D, Varikooty J, Simpson TL. Overnight corneal swelling with high and low powered silicone hydrogel lenses. J Optom. 2015;8(1):19-26.
-
8Maulvi FA, Soni TG, Shah DO. A review on therapeutic contact lenses for ocular drug delivery. Drug Deliv. 2016;23(8):3017-26.
-
9Montés-Micó R, Alió JL, Muñoz G, Charman WN. Temporal changes in optical quality of air-tear film interface at anterior cornea after blink. Invest Ophthalmol Vis Sci. 2004;45(6):1752-7.
-
10McAlinden C, Khadka J, Pesudovs K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt. 2011;31(4):330-8.
-
11Weschler S, Johnson MH, Businger U. In vivo hydration of hydrogel lenses: the first hour. Int Contact Lens Clin. 1983;10:349-52.
-
12Lewis JR, Knellinger AE, Mahmoud AM, Mauger TF. Effect of soft contact lenses on optical measurements of axial length and keratometry for biometry in eyes with corneal irregularities. Invest Ophthalmol Vis Sci. 2008;49(8):3371-8.
-
13Bendoriene J, Vogt U. Therapeutic use of silicone hydrogel contact lenses in children. Eye Contact Lens. 2006;32(2):104-8.
-
14Grentzelos MA, Plainis S, Astyrakakis NI, Diakonis VF, Kymionis GD, Kallinikos P, et al. Efficacy of 2 types of silicone hydrogel bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg. 2009;35(12):2103-8.
-
15Ozbek Z, Raber IM. Successful management of aniridic ocular surface disease with long-term bandage contact lens wear. Cornea. 2006;25(2):245-7.
-
16Chen D, Lian Y, Li J, Ma Y, Shen M, Lu F. Monitor corneal epithelial healing under bandage contact lens using ultrahigh-resolution optical coherence tomography after pterygium surgery. Eye Contact Lens. 2014;40(3):175-80.
-
17González-Méijome JM, Cerviño A, Peixoto-de-Matos SC, Madrid-Costa D, Jorge J, Ferrer-Blasco T. "In situ" corneal and contact lens thickness changes with high-resolution optical coherence tomography. Cornea. 2012;31(6):633-8.
-
18Cao HJ, Huang CJ, Shih PJ, Wang IJ, Yen JY. A Method of measuring corneal young's modulus. In: Goh J, Lim C, editors. 7th WACBE World Congress on Bioengineering. IFMBE Proc. 2015;52:47-50.
-
19Hamilton KE, Pye DC. Young's modulus in normal corneas and the effect on applanation tonometry. Optom Vis Sci. 2008;85(6):445-50.
-
20Jones IL, Warner M, Stevens JD. Mathematical modelling of the elastic properties of retina: a determination of Young's modulus. Eye (Lond). 1992;6(Pt 6):556-9.
-
21Aloy MÁ, Adsuara JE, Cerdá-Durán P, Obergaulinger M, Esteve-Taboada JJ, Ferrer-Blasco T, Montés-Micó, R. Estimation of the mechanical properties of the eye through the study of its vibrational modes. PLOS One 2017,vol. 12, issue 9, p. e0183892
Publication Dates
-
Publication in this collection
10 Jan 2019 -
Date of issue
Mar-Apr 2019
History
-
Received
06 Oct 2017 -
Accepted
22 June 2018